How AI Can Save You Thousands on Medical Bills: Beat USA Insurance Denials in 2025
#HealthInsurance, #AI, #MedicalBills, #InsuranceDenials, #PatientRights, #HealthcareAI, #AppealProcess, #USHealthcare, #PatientAdvocacy, #AIinHealthcare
How AI Can Save You Thousands on Medical Bills: Beat USA Insurance Denials in 2025
Discover how AI tools help USA patients and caregivers appeal health insurance denials and save thousands. Get a step-by-step guide to fight denials effectively in 2025. Start now!
How AI Can Save You Thousands on Medical Bills: Beat USA Insurance Denials in 2025
Introduction
Health insurance denials are a growing problem in the USA, affecting millions of patients and caregivers each year. In 2023, over 49 million insurance claims were denied, leaving patients with unexpected medical bills and delayed care. Appealing these denials can be daunting, but artificial intelligence (AI) offers a powerful solution. Tools like FightHealthInsurance.com use advanced technology to simplify the appeal process, helping you save thousands. This article provides a step-by-step guide for US patients and caregivers to use AI to fight insurance denials effectively in 2025 and beyond. Whether you’re facing a denied claim for surgery, therapy, or medication, this course will empower you to take control.
Why Health Insurance Denials Happen
Insurance denials occur for various reasons. The most common include:
Medical Necessity: Insurers may claim a treatment isn’t medically necessary based on their guidelines.
Policy Exclusions: Some treatments or services may not be covered under your plan.
Administrative Errors: Mistakes in coding or paperwork can lead to automatic denials.
Prior Authorization Issues: Treatments requiring pre-approval may be denied if the process wasn’t followed correctly.
These denials can lead to significant financial burdens, with patients facing bills ranging from hundreds to tens of thousands of dollars. Emotionally, denials can cause stress and delay critical care, impacting health outcomes. Understanding why a denial happens is the first step to fighting it effectively. By identifying the reason in your denial letter, you can build a strong appeal with the help of AI tools.
The Appeal Process Explained
Appealing an insurance denial involves two main stages: internal appeals and external reviews.
Internal Appeals: You submit a formal request to your insurance company to reconsider the denial. Standard appeals must be filed within 30 days, while expedited appeals for urgent care must be filed within 72 hours.
External Reviews: If the internal appeal is denied, you can request an independent review by a third party, typically within 45 days for standard cases or 72 hours for urgent ones.
The process requires gathering documents, drafting a compelling appeal letter, and meeting strict deadlines. Missing a deadline or submitting incomplete information can jeopardize your appeal. Fortunately, AI tools can streamline this process, making it faster and more accessible for patients and caregivers.
How AI Tools Help with Appeals
AI tools like FightHealthInsurance.com and Counterforce Health use natural language processing (NLP) and machine learning to analyze denial letters and generate personalized appeal letters. These tools can:
Read and interpret complex insurance denial letters.
Identify key issues, such as medical necessity or policy errors.
Draft professional appeal letters tailored to your case.
Suggest supporting documents, like medical records or doctor’s letters, to strengthen your appeal.
For example, FightHealthInsurance.com allows users to upload their denial letter, input relevant details, and receive a customized appeal letter in minutes. These tools are user-friendly, often free, and designed for patients, not just healthcare providers. They empower you to fight back without needing extensive legal or medical knowledge.
Step-by-Step Guide to Using AI for Appeals
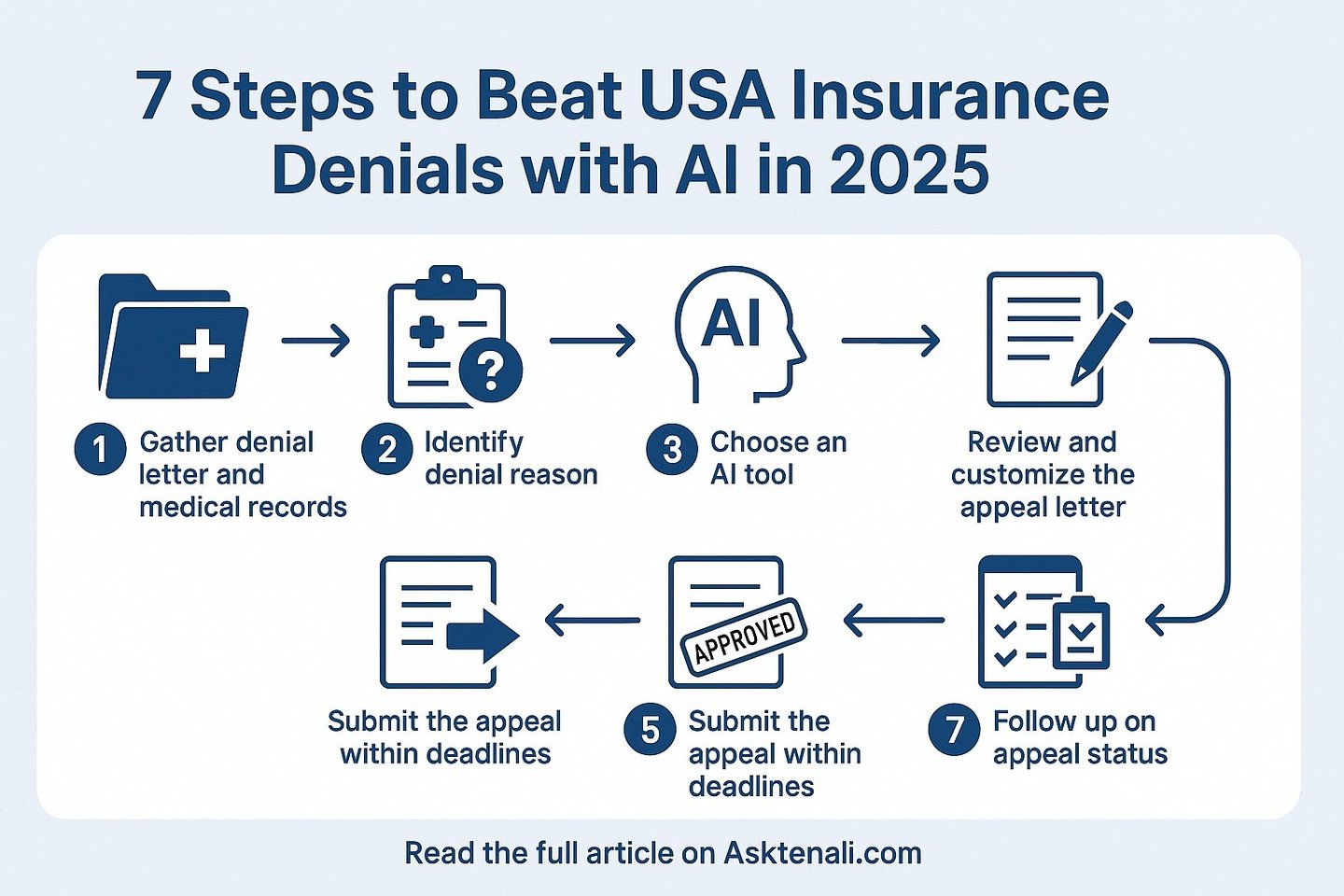
Here’s a detailed guide to using AI to appeal a health insurance denial in the USA:
Step 1: Gather All Necessary Documents
Start by collecting your denial letter, which explains why your claim was denied. Gather medical records, including diagnoses, treatment plans, and doctor’s notes. If applicable, include prior authorization documents or proof of coverage. Having all documents ready ensures the AI tool can generate an accurate appeal letter.
Step 2: Understand the Denial Reason
Read the denial letter carefully to identify the reason for the denial. Common reasons include “not medically necessary” or “service not covered.” If the letter is unclear, call your insurance company for clarification. Understanding the reason helps the AI tool address the specific issue in your appeal.
Step 3: Choose a Reputable AI Tool
Select an AI tool designed for patients, such as FightHealthInsurance.com or Counterforce Health. Check reviews to ensure the tool is reliable and user-friendly. Most tools are free or low-cost, making them accessible to everyone. Avoid tools meant only for healthcare providers, as they may be complex or expensive.
Step 4: Input Information into the AI Tool
Visit the AI tool’s website and follow the instructions. Upload your denial letter or enter the text manually. Provide additional details, such as your insurance policy number, medical records, and any relevant doctor’s notes. Accurate information is critical to generating an effective appeal letter.
Step 5: Review and Customize the Appeal Letter
The AI tool will generate a draft appeal letter based on your input. Review it carefully to ensure it includes all necessary details, such as the denial reason, supporting medical evidence, and a clear request for reconsideration. Add personal details, like how the denial affects your health or finances, to make the letter more compelling.
Step 6: Submit the Appeal
Follow your insurance company’s submission process, which may involve mailing, emailing, or uploading the appeal letter online. Include all supporting documents, such as medical records or doctor’s letters. Meet deadlines—30 days for standard appeals or 72 hours for expedited ones—to avoid dismissal.
Step 7: Follow Up on Your Appeal
Track the appeal’s progress, as insurers must respond within 30 days for standard appeals or 72 hours for expedited ones. If you don’t hear back, contact your insurance company to check the status. If the internal appeal is denied, request an external review for an independent evaluation.
Case Study: Jane’s Success with Physical Therapy
Jane, a 45-year-old from California, faced a denial for physical therapy after a knee injury. The insurer claimed it wasn’t medically necessary. Using FightHealthInsurance.com, Jane uploaded her denial letter and medical records. The AI tool generated an appeal letter highlighting her doctor’s recommendation and evidence of medical necessity. She customized the letter with details about her pain and mobility issues. Within 30 days, her appeal was approved, saving her $5,000 in out-of-pocket costs.
Case Study: Mark’s Home Health Care Appeal
Mark, a caregiver in Texas, had a denial for his mother’s home health care services due to a policy exclusion. He used an AI tool to draft an appeal letter, which included a doctor’s letter proving the service’s necessity. After submitting the appeal and following up, the insurer reversed the denial, covering $12,000 in care costs.
Legal and Ethical Considerations
When using AI tools, ensure the information you input is accurate to avoid errors in the appeal letter. Protect your privacy by using secure platforms that comply with data protection laws, such as HIPAA. AI tools are not a substitute for professional advice. If your case is complex, consult an attorney or patient advocate. Be aware that insurers also use AI to process claims, which can lead to bulk denials, so transparency in their processes is crucial.
The Future of AI in Healthcare Insurance
By 2025, AI tools for patients are expected to become more advanced, with improved NLP and integration with electronic health records. However, concerns remain about insurers using AI to deny claims without proper oversight. Advocacy for transparency and regulation will ensure fair use of AI on both sides. Patients can expect more tools like FightHealthInsurance.com to emerge, making appeals easier and more accessible.
Resources for Further Support
FightHealthInsurance.com: A free AI tool for generating appeal letters.
Healthcare.gov: Official resource for understanding appeal rights.
National Patient Advocate Foundation: Offers guidance and support for patients.
Counterforce Health: Another AI tool for appeal assistance.
Conclusion
Health insurance denials don’t have to be the end of the road. With AI tools, US patients and caregivers can fight back, save thousands, and access the care they need. By following the steps outlined—gathering documents, using AI to draft appeals, and submitting on time—you can navigate the complex insurance system with confidence. Start today and take control of your healthcare journey.
Key Citations
How to Appeal an Insurance Company Decision